Many health insurance plans cover shockwave tendonitis relief, but coverage varies. Pre-authorization or a referral may be needed. Out-of-pocket expenses differ between in-network and out-of-network providers. Comprehensive plans offer broader coverage for effective treatment without financial barriers. To secure reimbursement, review your policy, collaborate with healthcare providers, and understand the insurance carrier's claims process.
“Are you considering shockwave therapy for tendonitis but wondering about insurance coverage? This guide is your compass. Shockwave tendonitis relief has gained popularity as a non-invasive treatment option, but understanding insurance policies can be confusing. We demystify coverage by exploring common insurance plans and their stances on this innovative therapy. Learn essential steps to navigate claims effectively and maximize reimbursement for the shockwave tendonitis relief you deserve.”
- Understanding Shockwave Tendonitis Relief Coverage
- Common Insurance Plans and Their Policies
- Navigating Claims: Steps to Ensure Reimbursement
Understanding Shockwave Tendonitis Relief Coverage

Understanding Shockwave Tendonitis Relief Coverage
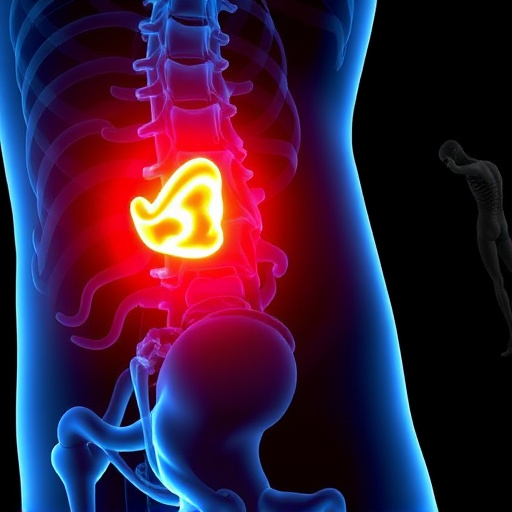
When considering shockwave tendonitis relief as a treatment option, it’s natural to wonder about insurance coverage. Many health insurance plans in today’s digital era do include provisions for non-invasive treatments aimed at pain management, including shockwave therapy for tendonitis. However, the level of coverage can vary significantly from one plan to another. It’s important to note that specific policies may require pre-authorization or a referral from your primary care physician before approving this type of treatment, especially if it’s considered experimental or not commonly prescribed for pinched nerve relief.
Delve into the specifics of your insurance plan to comprehend the extent of coverage. Typically, shockwave tendonitis relief is seen as a cost-effective and relatively low-risk procedure compared to surgical options. As such, many plans are now including it in their benefits packages. In terms of out-of-pocket expenses, co-pays and deductibles may apply, so reviewing these details with your insurance provider is crucial. Remember that the goal of shockwave therapy is to offer a non-invasive treatment solution for pain management, potentially revolutionizing the way tendonitis is addressed without the need for extensive interventions.
Common Insurance Plans and Their Policies

Many insurance plans, both private and group-based, cover shockwave tendonitis relief procedures to varying degrees. This is because these treatments have gained recognition for their effectiveness in managing musculoskeletal injuries, including tendinitis. When it comes to specific coverage, policies often include terms like ‘in-network’ and ‘out-of-network’ providers, which can significantly impact patient costs. In-network providers are typically preferred as they usually require lower out-of-pocket expenses, while out-of-network services might be more expensive but can still be covered with the right authorization.
Insurers often differentiate between diagnostic and treatment costs. Shockwave therapy for tendonitis relief is generally considered a treatment option and is therefore subject to coverage limits or specific criteria. Personalized treatment plans, which include shockwave therapy, may be viewed as specialized care and could be more extensively covered by plans that offer comprehensive benefits for musculoskeletal healthcare. This ensures patients can access effective headache relief and other related treatments without facing substantial financial burdens.
Navigating Claims: Steps to Ensure Reimbursement

Navigating Claims: Steps to Ensure Reimbursement for Shockwave Tendonitis Relief
When seeking shockwave tendonitis relief, understanding your insurance coverage is crucial. The process of filing a claim can seem daunting, but by following structured steps, you can ensure a smoother journey towards reimbursement. First, review your policy documents carefully to identify specific clauses related to chiropractic care and innovative treatments like shockwave therapy. Many insurance plans do cover shockwave tendonitis relief, recognizing its effectiveness in injury rehabilitation.
Next, consult with your healthcare provider to obtain the necessary diagnostic reports and treatment records detailing your condition and the recommended shockwave therapy. These documents are vital for substantiating your claim. Then, contact your insurance carrier directly and inquire about their specific procedures for filing a claim. Be prepared to provide them with all required information and documentation. This proactive approach will help streamline the claims process and increase the likelihood of successful reimbursement for your shockwave tendonitis relief treatment.
Shockwave tendonitis relief, an innovative treatment option for those suffering from chronic tendon pain, is increasingly recognized as a valuable healthcare solution. While coverage varies across insurance plans, understanding your policy and taking proactive steps can facilitate reimbursement. By familiarizing yourself with your insurer’s policies, following proper claim navigation procedures, and providing comprehensive documentation, you can ensure access to this potentially life-changing treatment. Remember, each step towards effective shockwave tendonitis relief is a step towards improved mobility and overall well-being.